The role of social prescribing in relieving suffering
England's citizens are suffering.
Hammered by the COVID-19 pandemic and its associated lockdowns as well as the more recent cost of living crisis, made worse by the war in Ukraine, systemic shocks are negatively impacting the wider determinants of health that impact wellbeing and livelihoods.
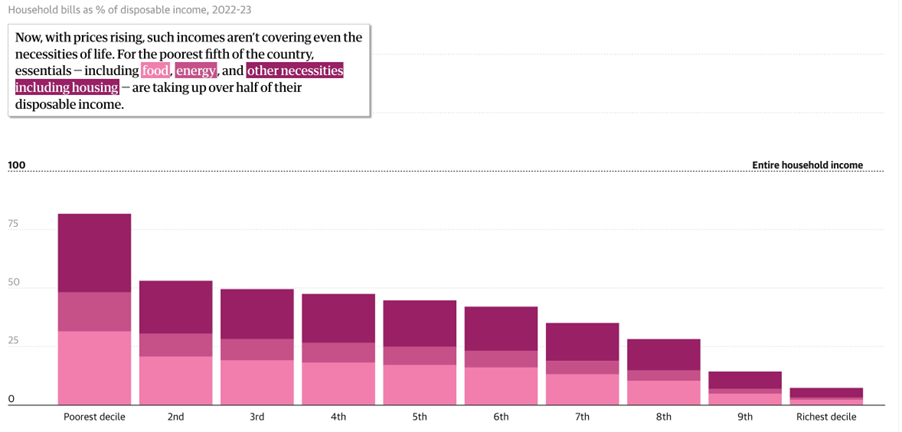
UK consumer confidence falls to the lowest level since records began1
With prices rising, such incomes aren't covering even the necessities of life. For the poorest fifth of the country, essentials – including food, energy and other necessities including housing – are taking up over half of their disposable income:2
In the face of these pressures, reverting to medicalisation will not help suffering citizens or our already overstretched health and care systems. This realisation is at the core of the Beyond Pills campaign, which was launched in the House of Lords on June 17, 2022, and aims to push the drive towards using non-medical interventions, like social prescribing, to support citizens and health and care systems to address non-medical needs.3
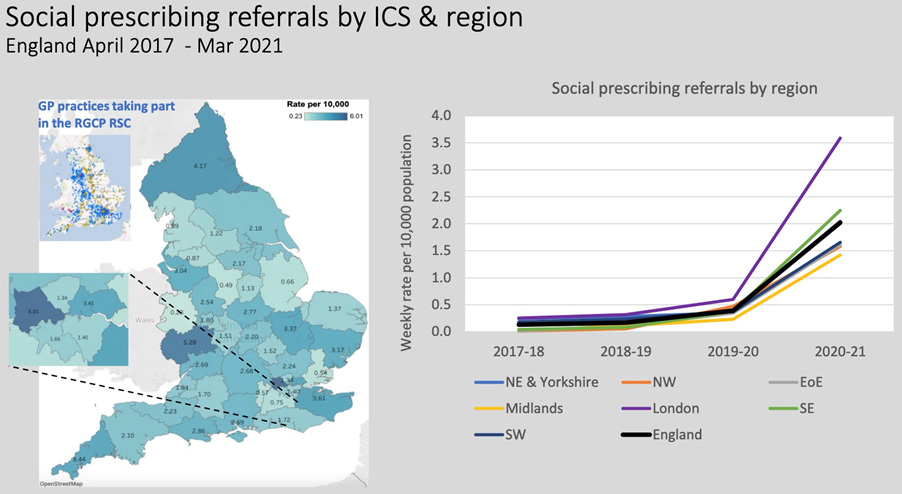
To explorate the use and impact of non-medical interventions like social prescribing, NHS England and NHS Improvement commissioned the Royal College of GPs and the University of Oxford to develop four free and public observatories to track social need as well as the use of non-medical interventions, including social prescribing4:
https://orchid.phc.ox.ac.uk/index.php/social-prescribing/.
The observatories use data from the RCGP Research & Surveillance Centre (RCGP RSC), which was established in 1967 and currently collects data from over 1700 nationally representative GP practices across England. The dataset consists of pseudonymised extracts of data from GP practice electronic health records.5
Increase in and variation in the use of social prescribing
- Recorded use of personalised care in primary care is growing rapidly and has remained at a high level since the pandemic. Most of this increase relates to social prescribing.
- Recorded use of some types of support (eg physical activity referrals) dropped during the COVID-19 pandemic. This may reflect the pressures on primary care, a reduction in provision of activities and the effects of the lock-down.
- Recorded rates of social prescribing referrals vary greatly across England - from 0.23-6.01 per 10,000 population per week – an approximately 25-fold variation (see above).
- The variation between regions widened during 2020-21 (see above).
Social prescribing is not evenly distributed
- We found large differences in recorded use between groups for non-medical interventions like social prescribing.
- People over 65, people of White ethnicity and women are the most likely to have a recorded intervention. Children, younger adults, men, and people from non-White backgrounds currently have fewer recorded interventions.
- People living in the most deprived neighbourhoods appear slightly more likely to have a non-medical intervention, but the difference is small and not statistically significant.
These findings are promising but they also raise some concerns and questions that could help us explore ways to more formally integrate interventions like social prescribing into healthcare systems to support citizens suffering from non-medical needs.
- It is important to note that our findings do not yet point to or constitute evidence of the impact of non-medical interventions. More work is needed to support the generation of evidence on how these types of interventions can be used to improve health and wellbeing outcomes for patients, reduce health inequalities, address unmet needs and deliver wider benefits to the NHS.
- As part of the drive towards integrated care, as delivered by ICSs, more consultation is needed with communities to co-produce mechanisms to strengthen links between primary care and local authorities to address social exclusion and investigate barriers to accessing non-medical interventions.
- More support and guidance is needed on coding so that demographic data, presenting needs of individuals (linked to social determinants of health) and the components of non-medical interventions are consistently recorded in electronic health records across all settings.
Written by Dr Anant Jani
References
- 1.https://www.ft.com/content/5c26babd-fa10-4ca7-a7fd-085b1f10a626
- 2.https://www.theguardian.com/business/ng-interactive/2022/jun/21/cost-of-living-crisis-uk-households-charts-inflation
- 3.https://www.ipmcongress.com/whole-person-health-conference-draft/beyond-pills-is-over-medicalisation-over-moving-towards-a-less-medicalised-model-of-healthcare
- 4.https://orchid.phc.ox.ac.uk/index.php/social-prescribing/
- 5.https://orchid.phc.ox.ac.uk/wp-content/uploads/2021/08/Health-inequalities-and-personalised-care-in-England-Apr-2017-Mar-2021.pdf
- 6.Preparing for COVID-19's aftermath: simple steps to address social determinants of health. https://pubmed.ncbi.nlm.nih.gov/32314660/
When you subscribe to the blog, we will send you an e-mail when there are new updates on the site so you wouldn't miss them.


Comments