Social prescribing: why I’m flying the flag in medical school
People on the whole are quite complex.
In medicine we tend to see a snapshot of a tired, ill patient and then fight against the ticking clock to match them with whatever medicine, treatment or referral best suits their disease. It's a healthcare model that reacts to disease states after they have developed and would be adequate if illnesses existed in isolation.
However, we know that's not true. Developing research on the gut-brain axis, the microbiome, physiology in depression and even, more recently, Covid-19 has added evidence to what we suspected: overall well-being is dependent on a careful equilibrium of interconnected systems. What's more, every individual has a unique set of systems; metabolising drugs, genetic predispositions, gut flora, thought processes- these complex systems can differ hugely between two patients with the exact same illness.
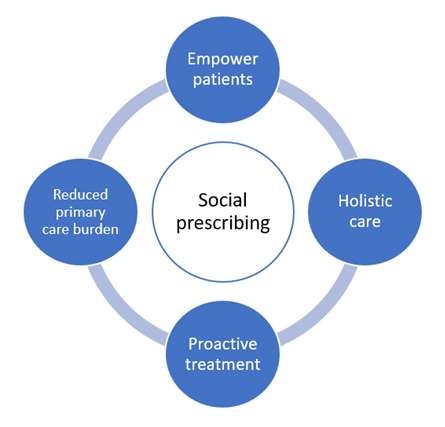
This is why I support social prescribing: it is a system that provides tailored, holistic treatment to patients whilst reducing the burden on primary care services. As a medical student, I've seen many patients whose needs extend beyond drugs and surgery: enabling them to access services in the community can meet these needs, restoring independence, positivity and equilibrium.
Social prescribing has many potential benefits, but the four that I think are the most useful are presented here. With an increasingly ageing population, social isolation is becoming more prevalent.
How will I use it to help my patients?
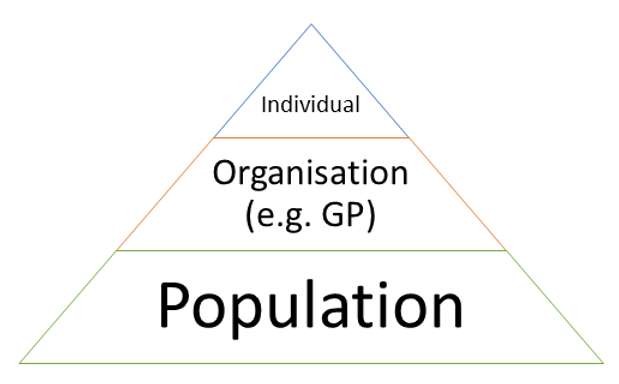
I like to think of this at three levels: the individual, the organisation and the population. Social prescribing has the potential to make improvements on all three levels, which could have profound impacts on healthcare as a whole.
Social prescribing has the potential to help the individual (the patient), the organisation (primary care services, hospitals) and the population as a whole. Reducing overall disease burden should always be a goal in healthcare.
The individual
Patients frequently have needs beyond the clinic. Although my naive student brain hopes that I will take the time to explore their diet, exercise, pain, wider relationships and general life, I know that this is not always a realistic achievement.
Even the most compassionate, knowledgeable doctors that I've observed can struggle with a full patient list and an hour delay in clinic.
By connecting these patients with link workers, who can then signpost them to social initiatives, I hope that these wider needs will be met. Exercise classes could be used to improve weight management and symptoms, for pacing in chronic pain conditions or as a boost to mental health. Relaxation services such as art, yoga and music therapy could provide much needed solace and reflection. Cooking classes and nutrition services could improve weight and symptom control. From a wider point of view, patients experiencing social isolation or health inequalities could be given much-needed access that otherwise would not be met.
The added value lies in patient choice (especially with self-referral), which would enable me to connect my patients with the services they want as an individual. Adherence to programmes is a common barrier to success and so I would hope the empowerment would enable the patients to take control of their well-being and feel the accountability that brings success.
The organisation
With one in five GP visits for non-clinical issues, an ageing population with co-morbidities and increased national (and worldwide) disease burden, there is significant stress on healthcare services.
I hope that by championing social prescribing and utilising it in my healthcare organisation (which one is, as of yet, undecided!) I can help to reduce the workload and strain. The result would be a more motivated workforce with better mental health, freeing up of healthcare services and the ability to focus on improving systems and other problems. Secondary care services are also positioned to develop social prescribing pathways, which could have the added benefit of improving the connection between primary and secondary healthcare.
The evidence seems to support this: a summary by the University of Westminster suggests that GP consultations are reduced by an average of 28% (and A&E visits by 24%) for a patient that accesses social prescribing services. The implications of these figures, not just on cost but on wider points such as well-being of staff are too important to dismiss.
Population
Looking at the top ten global diseases from the World Health Organisation shows an astounding need to address diet, exercise and general "modifiable" risk factors. There are obvious diseases, such as ischaemic heart disease and diabetes, but also those less widely known to be connected to diet and exercise, such as Alzheimer's disease (also linked to social isolation). More recently with the Covid-19 pandemic, it has been shown that patients with metabolic syndrome are at increased risk for infection and severe complications.
In addition, the NHS long term plan has laid out the intention to extend personalised healthcare and to focus more on preventative services and unmet healthcare needs. Social prescribing could have a positive effect on the population by reducing risk factors (via diet, exercise and improved mental health) and addressing the unmet healthcare needs of vulnerable patients, such as those in poverty or adolescent mental health patients.
Final thoughts
Although most of my colleagues are very supportive of my interest in social prescribing, we still have to tackle the common problems- "isn't it a bit obvious? You just tell them to eat well and exercise? Do we really need services for this? It's beyond a Cambridge medic to be focusing on soft science!"
I hope that more research will be conducted on the benefits of social prescribing and it will become more of a complement to medical school curricula. For now, I'll continue to explore it and educate my colleagues (and some superiors!) but hopefully I'll be able to stubbornly hold onto my naivety, until I'm talking to my own patients about social prescribing. Watch this space.
When you subscribe to the blog, we will send you an e-mail when there are new updates on the site so you wouldn't miss them.



Comments